WHO conducted a key informant survey among ministry of health officials in five regions to assess the impact of the COVID-19 pandemic on up to 25 essential health services in various countries. Most of the countries surveyed reported minor to severe disruption in essential healthcare services. Here is a review.
Healthcare services around the world have faced numerous challenges related to overstretched capacity and fragmentation due to the COVID-19 pandemic. The World Health Organisation (WHO) has released a series of studies assessing the impact of the COVID-19 pandemic on global health goals, highlighting the urgent need to work towards stronger, more equitable health care facilities and information systems.
In the context of India, some of our earlier stories have highlighted the impact of the pandemic on health facilities, education, aspects of the economy such as vehicle registration, air passenger traffic, and status of Indian states in terms of employment and migration.
Impact of the COVID-19 pandemic on essential health services
WHO conducted a key informant survey among the ministry of health officials in five regions to assess the impact of the COVID-19 pandemic on up to 25 essential health services in various countries. Two rounds of the Pulse survey on continuity of essential health services during the COVID-19 pandemic have been published in August 2020 and April 2021. The results indicate that even robust health systems can be rapidly overwhelmed and compromised by a COVID-19 outbreak, reinforcing the need for strategic adaptations to ensure the maintenance of essential health services.
The pandemic is testing all national health systems, with an impact on essential health service delivery and utilization in almost every country in the five WHO regions surveyed. The findings show that one year into the pandemic, health systems around the world are still being challenged. Nearly every responding country reported disruptions to one or more essential health services, and disruptions were reported across all service delivery platforms and health areas. The impact may be felt beyond the immediate pandemic as, in trying to catch up on services, countries may find that resources are overwhelmed, as per the findings of the survey.
The type and number of services affected by the COVID-19 pandemic varied between countries and regions.
- 94% of participating countries reported disruptions in at least one essential health service.
- 34% of countries reported disruptions in over half of services (with approximately 9% of countries reporting disruptions in 75–100% of services and 25% reporting disruptions in 50-74% of services).
- 29% of countries reported disruptions in 25–49% of services.
- 32% reported disruptions in less than 25% of services.
- Only 6% of countries reported no service disruptions.
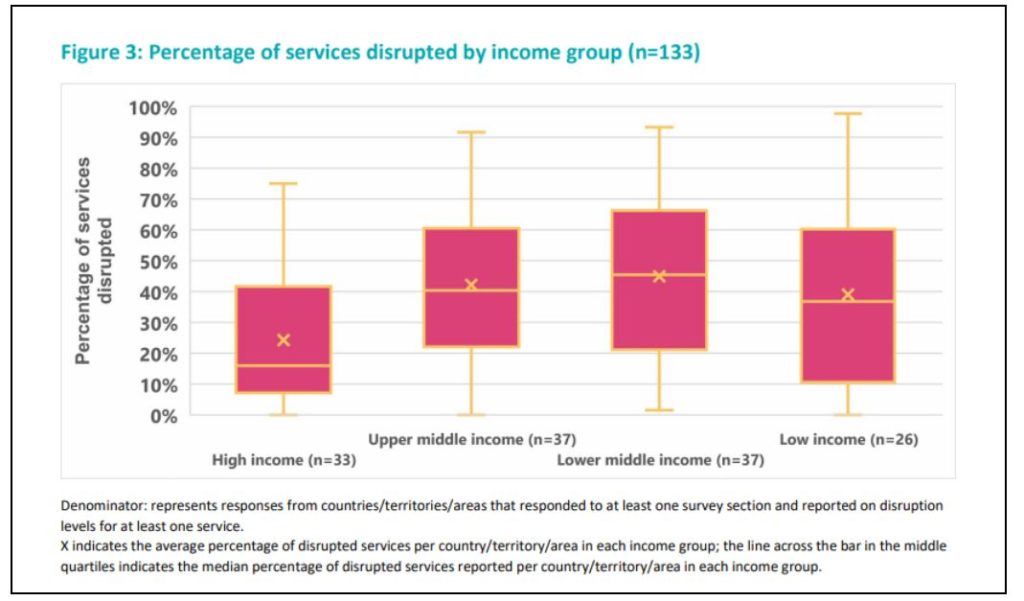
Overall, wide variation is seen in the level of disruption reported across countries within each region and income group. Countries in high-income groups reported fewer disruptions compared to countries in other income groupings.
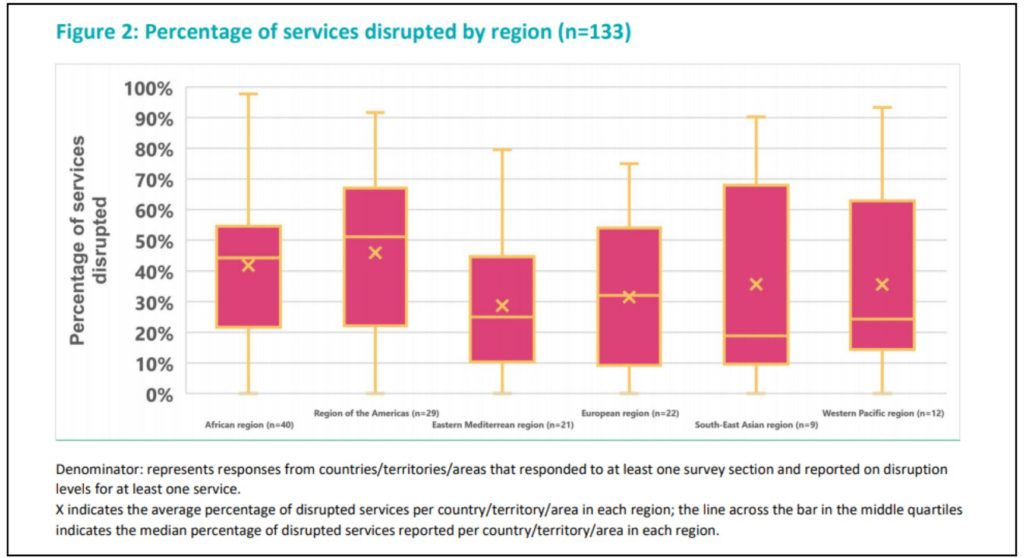
Overall, countries in the WHO Region of the Americas reported the highest average percentage of services disrupted per region, although these findings should be interpreted with caution, given the varied response rates across regions.
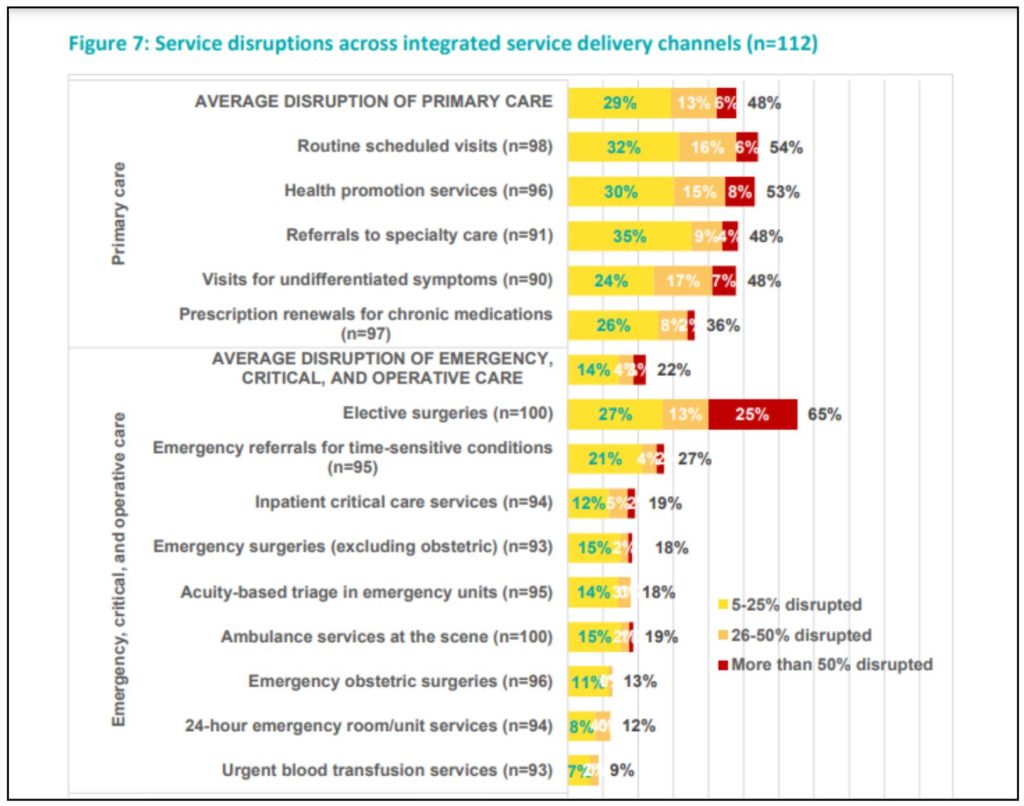
Primary care and rehabilitative, palliative and long-term care are predominantly affected. On average, 35% of 112 countries reported disruptions across all service delivery channels. Primary care sits at the foundation of achieving universal health coverage (UHC), and any disruptions in this setting can cause severe impact across the health system for service delivery and the overall health and well-being of patients. Other essential primary care services, including referrals to specialty care (48% of 91 countries) and visits for undifferentiated symptoms (48% of 90 countries), were also disrupted in nearly half of the countries.
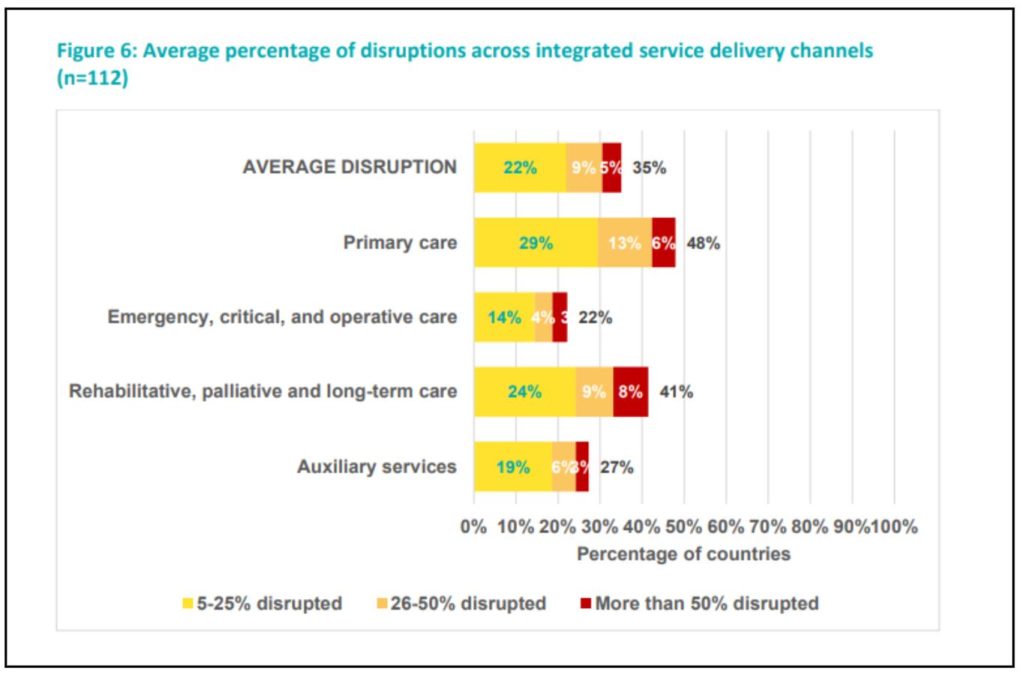
Disruptions to potentially life-saving emergency, critical and operative care interventions are of urgent concern as any disruptions in these areas can cause severe near-term indirect consequences on health outcomes. Substantial disruptions have been reported across various emergency services, as shown in the graph below. More than half of countries reported disruptions to rehabilitative services, and more than one-third of countries reported disruptions to palliative and long-term care services. Auxiliary services, including laboratory services and radiology services, were disrupted in 26 (27%) and 27 (28%) countries respectively.
Further, on average, 35% of countries reported disruptions across reproductive, maternal, newborn, child and adolescent health (RMNCAH) and nutrition services. The most frequently disrupted services were family planning and contraception services and management of moderate and severe malnutrition, both of which were disrupted in more than 40% of reporting countries.
The collapse of essential health services – including health promotion, preventive services, diagnosis, treatment and rehabilitative and palliative services – is likely to have serious adverse health effects, especially on the most vulnerable populations.
The results also shed light on the importance of responsive health policy planning and action, as countries must continue to orient health strategies according to the current and rapidly changing priorities and needs of populations to ensure continued provision of and access to care. The findings also highlight the need to ensure that COVID-19 control strategies are in balance with other health priorities.
Disproportionate Impact on Vulnerable Populations
Despite recent global health gains in the previous decades across the world, people continue to face complex, interconnected threats to their health and well-being rooted in social, economic, political, and environmental determinants of health.
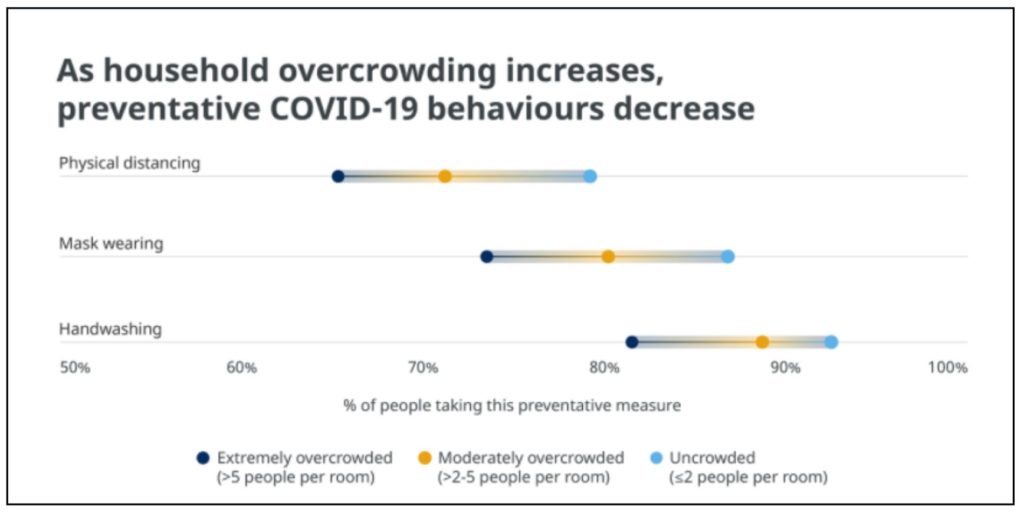
Data from the COVID-19 World Symptoms survey shows a decline in preventive behaviours such as physical distancing, mask-wearing and hand washing as household overcrowding increases. Among people living in uncrowded households, 79% reported trying to physically distance themselves compared with 71% in moderately overcrowded and 65% in extremely overcrowded households. Similar trends were observed for handwashing and mask-wearing, underscoring vulnerabilities due to socioeconomic status.
Gaps in Health Information Systems
The pandemic has also revealed significant gaps in country health information systems. A first of its kind Score Global Report on Health Systems and Capacity 2020 assess health information systems in 133 countries, covering 87% of the global population. The report reveals that only half of countries include disaggregated data in their published national health statistical reports.
Among several key findings, the income divide between high and low-income countries is reflected in the lack of health information system capacity to address fundamental areas such as the registration of births, deaths and causes of death. While some countries have achieved sustainable capacity in some key areas, no country has a fully mature system capable of meeting their evolving needs for health information. For instance, while 97% and 82%, respectively, of high-income and upper-middle-income countries, have well-developed and higher capacity for death registration, only 27% of lower-middle-income countries and no low-income countries achieve the same capacity.
Focused spending on key programme areas such as immunization and tuberculosis, has improved their data availability but has not uniformly strengthened the reporting system. For example, less than 50% of countries have data available for mental health disorders compared to almost 100% of countries that have data for immunization and tuberculosis.
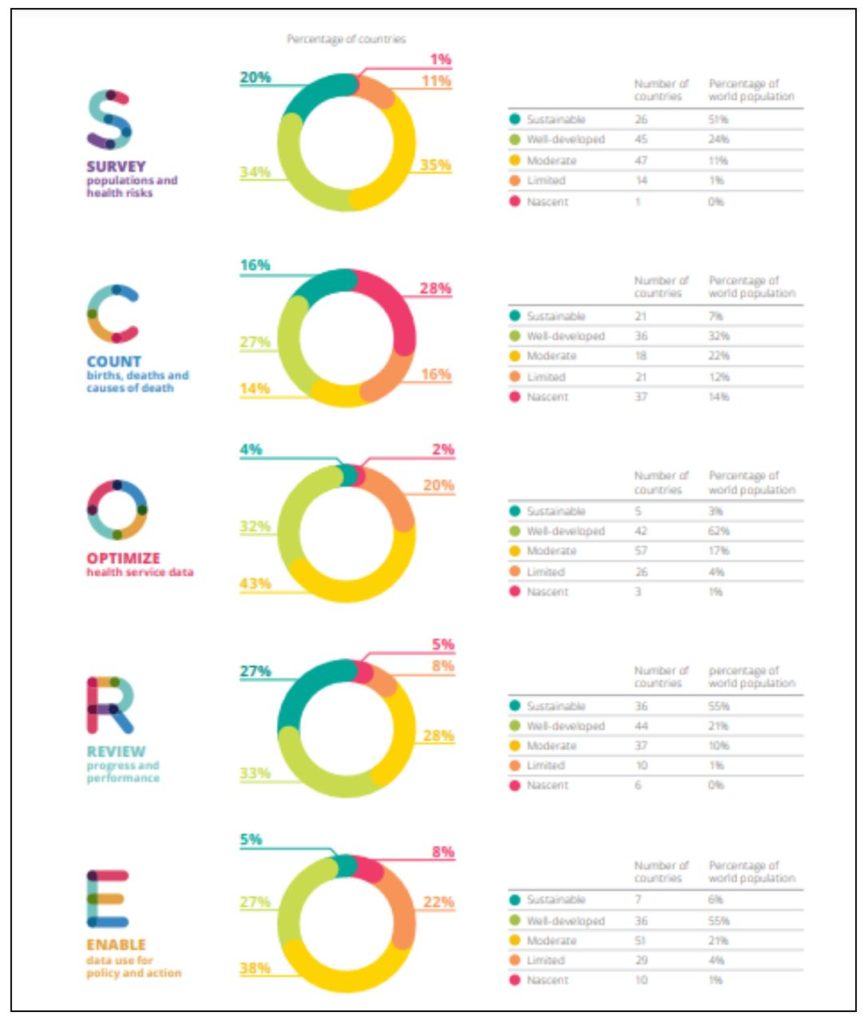
The report also indicates that data quality is a critical issue for health facilities with about 40% of countries not showing clear evidence that data quality assurance processes have been followed for their published health facility data. There is legitimate concern about the quality of cause-of-death data. Only 28% of countries have less than 10% ill-defined cause-of-death codes. The remaining 72% either do not record cause-of-death data using International Classification of Diseases (ICD) codes, or have more than 10% ill-defined cause-of-death codes.
Need for robust health facilities and information systems
One of the most important takeaways from these surveys is weaker health systems risk jeopardizing hard-won health and development gains made in recent decades. As the pandemic is likely to ebb and flow over the coming months, real-time monitoring of changes in health service delivery and utilization is needed.
Featured Image: COVID-19 Impact on essential healthcare services


