In the wake of the challenges posed by COVID induced lockdown, telemedicine has emerged as a solution to provide healthcare facilities. The government has also recently issued guidelines for telemedicine practice. What is in these guidelines? Here is an explainer.
With the advancements made in Information and Communication Technology, often abbreviated as ICT, people’s lives have changed drastically. Even amidst the COVID-19 pandemic that is wreaking havoc across the globe, ICT is playing a vital role in navigating through the situation. Telemedicine or telehealth is one such technological intervention which has gained momentum during COVID induced lockdown.
In India, the Ministry of Health issued guidelines on telemedicine practices on 25 March 2020, the first day of national lockdown. It was prepared in collaboration with NITI Aayog. Not only does this prove useful at a time when there are restrictions on movement, but also helps in reducing crowd in hospitals, bringing down the risk of infection. Later, on 12 May 2020, the government published the guidelines in the gazette, incorporating the same into the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002. This means consultation through telemedicine by a Registered Medical Practitioner (RMP) under the Indian Medical Council Act, 1956 is now permitted as per the notified guidelines. The notification also states that these guidelines are not applicable to the use of digital technology to conduct surgical or invasive procedure remotely.
Telemedicine has been given a legal status in India
The guidelines have adopted the definition of telemedicine as given by World Health Organization (WHO). The definition is as follows,
‘The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.’
Telehealth is a broader term which includes health and health related services including telemedicine. It is defined as,
‘The delivery and facilitation of health and health-related services including medical care, provider and patient education, health information services, and self-care via telecommunications and digital communication technologies.’
For now, Registered Medical Practitioners are authorized to practice telemedicine
To begin with, only RMPs are authorized to practice telemedicine. An RMP is any person who is enrolled in the State Medical Register or Indian Medical Register under the Indian Medical Council Act. All ethical norms and standards applicable for in-person consultation are also applicable in case of telemedicine practice.
Currently, RMPs must follow the guidelines issued by the Board of Governors (BoG) of MCI. However, an online course of three years duration will soon be notified by BoG. Once the course is approved and becomes operational, only those RMPs who complete the course will be allowed to consult online.
Any mode of communication can be used
Consultation can take place through any mode of communication such as audio, video, or texts. A person can access the service through any means such as WhatsApp, Facebook Messenger, Hangouts, among many others. There are also dedicated applications and websites for telemedicine services. Depending on the case, it is up to the RMP to decide whether online consultation will suffice or if an in-person consultation is required. Even the mode of communication is left to the discretion of the RMP which in turn is dependent on the patient’s diagnosis/treatment.
Consultations should not be anonymous, and patient’s consent is important
No telemedicine consultation should be anonymous as per the guidelines. While the RMP must verify and confirm a patient’s basic details such as name, age, contact details, address, etc., the patient should also be provided with the RMP’s credentials and basic contact information. In other words, both patient and the RMP need to know each other’s identity.
Patient’s consent is another important issue addressed in the guidelines. If a patient initiates the consultation, it means they have given their consent. Suppose an RMP initiates consultation, then an explicit consent must be recorded from the patient.
There are two types of consultation, first consultation and follow up consultation. First consult is when a patient is consulting the RMP for the first time, or after more than six months from the previous consultation, or if they consult the RMP for a different illness. Follow up consultation is when a patient consults the same RMP for the same health condition or within six months from previous consultation.
RMPs can impart health education, counsel, or prescribe medicines as per requirement
Based on diagnosis, the RMP can provide health education such as advice on habits and hygiene practice, counselling like food restrictions and giving out do’s and don’ts. Prescription of medicines can be done only if the RMP is sure that enough relevant information has been collected. The Government of India will notify from time to time, the list of medicines which can be prescribed online.
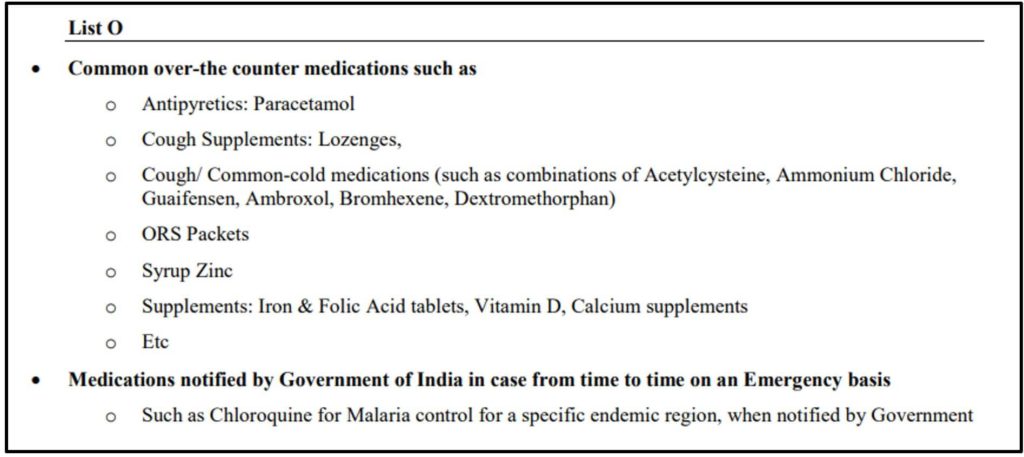
There are four categories of medicines based on potential for abuse
There are four categories of medicines which have been listed out – List O, List A, List B, and Prohibited List.
List O consists of medicines which are safe to be prescribed through any mode of tele-consultation, audio, video, or text. The list consists of ‘over the counter’ medicines such as paracetamol, ORS solutions, Cough syrup, etc.
List A comprises of medicines which can be prescribed for patients in their first consultation which should be through video, or for re-filling or re-prescribing in case of follow up consultation. The list would include those medicines which are safe and have a low potential for abuse.
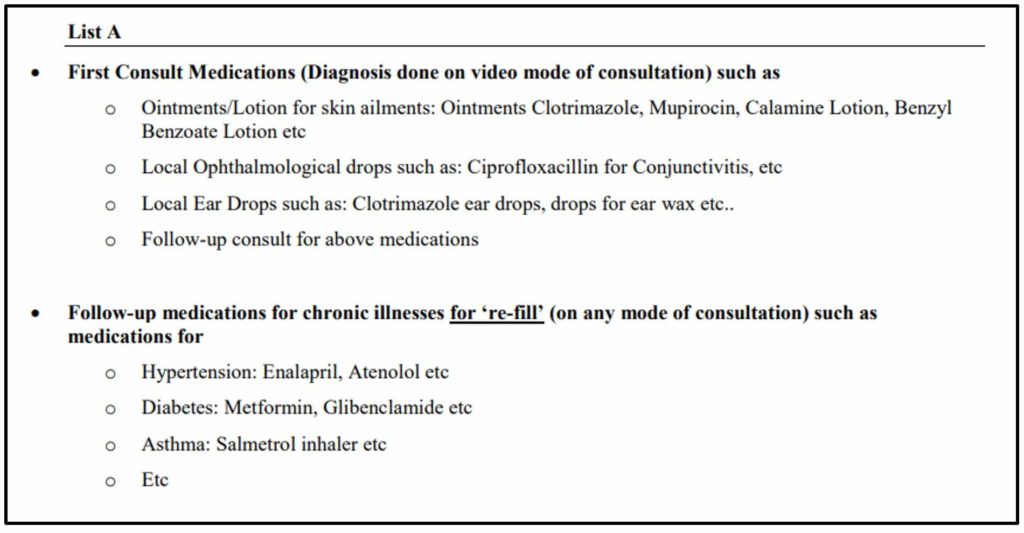
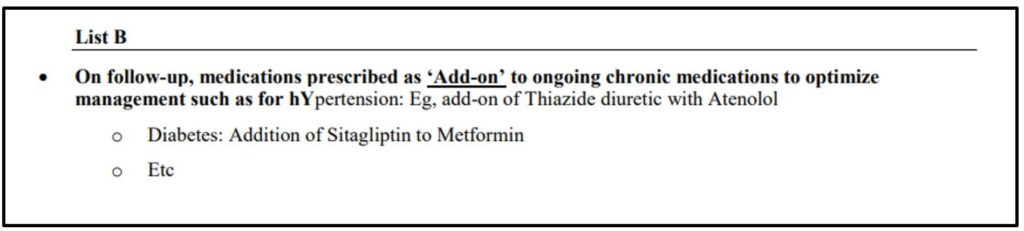
List B consists of medication which can be prescribed to a patient who is undergoing follow up consultation in addition to those medicines which were already prescribed for the same medical condition.
Prohibited list comprises of medicines which have the potential to be abused and affect the person or society. These cannot be prescribed through tele-consultation. Medicines listed in Schedule X of Drug and Cosmetic Act and Rules or any Narcotic and Psychotropic substance listed in the Narcotic Drugs and Psychotropic Substances, Act, 1985 fall under this list.
The RMP must send a copy of the signed prescription to the patient via email or message.
Legal provisions of IT Act, IMC Act, and privacy laws/rules are applicable
The IT Act and data protection & privacy laws/ rules issued by the government are applicable in case of telemedicine practice as well. Protection of patient privacy and confidentiality are as per the IMC Act. However, if the breach of confidentiality is due to technology breach or by someone else, RMP will not be held responsible.
RMP must maintain a record of telemedicine interaction such as phone logs, chats, videos, etc. The documents and reports submitted by the patient during consultation, prescription copies must also be retained by the RMP.
The patient must be provided an invoice or receipt for the fee charged for the consultation. Fee applicable here is just as that applicable for an in-person consultation.
Telemedicine service has the potential to address some major problems in healthcare
The COVID-19 pandemic has posed a challenge in extending normal healthcare services. On one hand, existing resources are being diverted towards containing the virus and treating the affected. On the other hand, even existing health facilities are not working normally because of the restrictions in place. Thus, promoting telemedicine fills the critical gap, especially for those who are in need of a doctor consultation.
Telemedicine applications in mobile phones and websites are already available in India. Even major hospital chains in India provide online healthcare services. One main advantage of telemedicine is that it avoids self-medication. It also acts as an enabler and if channelled properly, can help medical services reach remote areas too. There are separate guidelines for telemedicine practice among AYUSH health practitioners.
However, one has to understand that not all diagnosis or treatment can be done online. The mode of communication & the ability to articulate the symptoms also plays a major role. For instance, if e-mail is used as the mode of communication, the understanding of the patient’s condition by the RMP will solely depend on the articulation in the mail. Similarly, technological limitations such as network speed etc. can also affect telemedicine practice.
Featured Image: Telemedicine guidelines


