Recently, the CAG tabled the performance audit report on the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY). The CAG’s performance audit report of AB-PMJAY covered five different aspects of the scheme that highlighted multiple discrepancies. The report also made important recommendations. Here is a review.
Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PMJAY) is a flagship health scheme launched by Government of India in 2018. It aims to provide ‘Universal Health Coverage’ to the poor and vulnerable sections of the society by ensuring access to healthcare services and reduce the out-of-pocket medical expenditure. PMJAY provides a health cover up to Rs. 5 lakh per family per year, for secondary and tertiary care hospitalization services. It provides cashless and paperless access to services for the beneficiaries at the point of service.
Recently, the Comptroller and Auditor General of India (CAG) tabled the performance audit report on the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY). The CAG’s performance audit report of AB-PMJAY covered five different aspects of the scheme – Beneficiary Identification and Registration, Hospital Empanelment and Management, Claims Management, Financial Management and Monitoring & Grievance Redressal. The sample size of the Performance audit was 964 hospitals across 161 districts in 28 States. Here is a review of the findings, observations, and recommendations from the CAG report on PMJAY.
Obsolete and erroneous information in the Database used for Beneficiary identification.
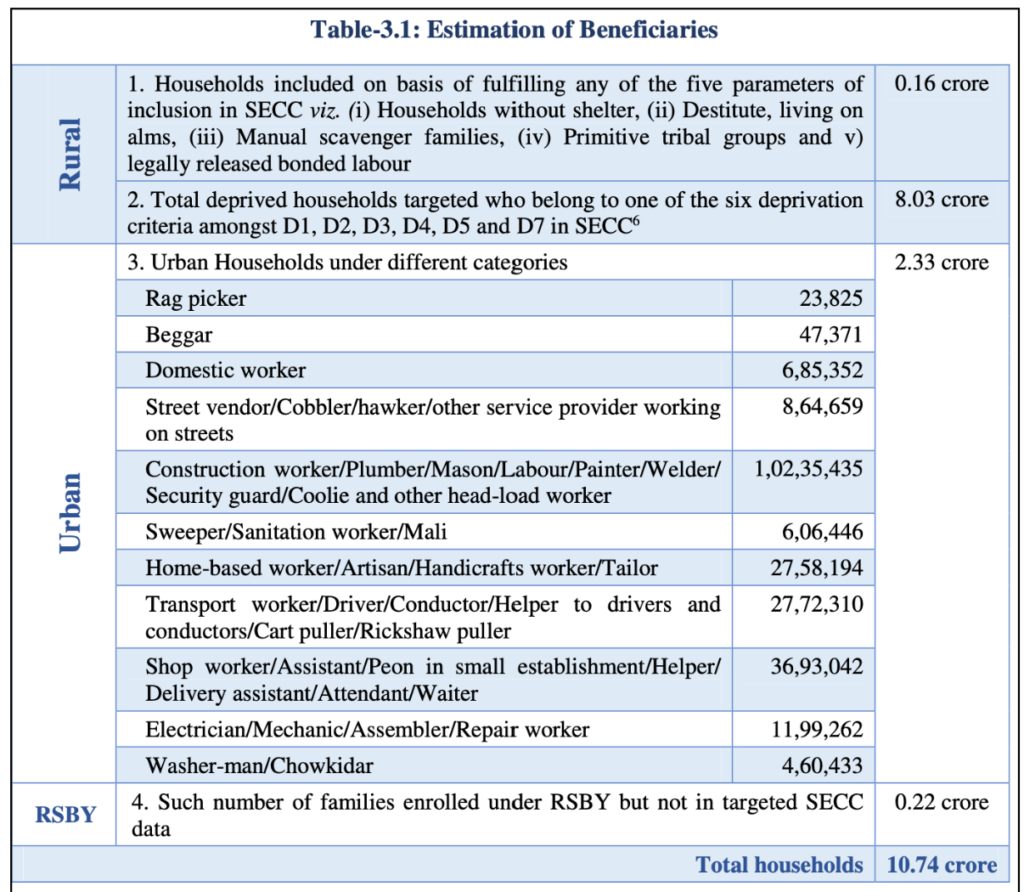
One of the key focus areas of the audit was around the process of identification and registration of the beneficiaries. Based on the deprivation and occupational criteria of the Socio-Economic Caste Census, 2011 (SECC-2011), PM-JAY envisages to cover 10.74 core families.
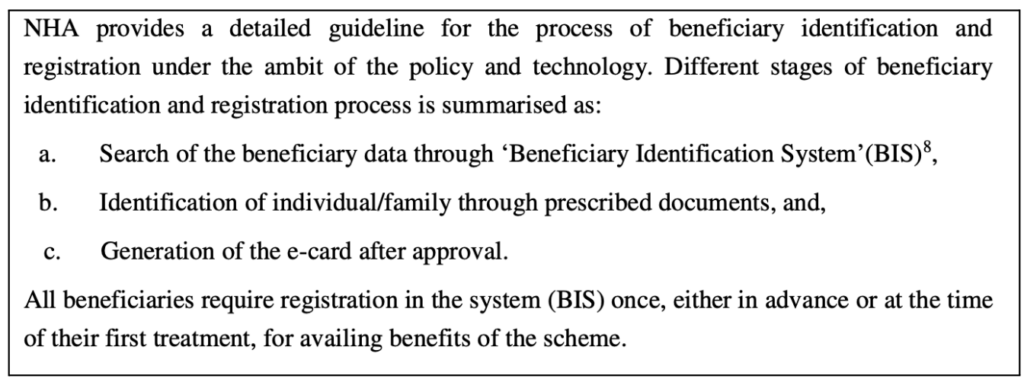
States are also given the flexibility to use their own database for the implementation of PMJAY. This was expanded to 12 crore families in Janaury’2022. The National Health Authority (NHA) laid out process for identification of beneficiaries.
CAG’s report noted some inconsistencies across few states in flagging the beneficiaries eligible for central schemes and those that are part of the state schemes. It has suggested a review of the beneficiary registration system to ensure eligible beneficiaries are covered and a clear identification of beneficiaries under Central and State Schemes is available.
Apart from beneficiary identification, the report highlighted the following observations regarding the Registration process.
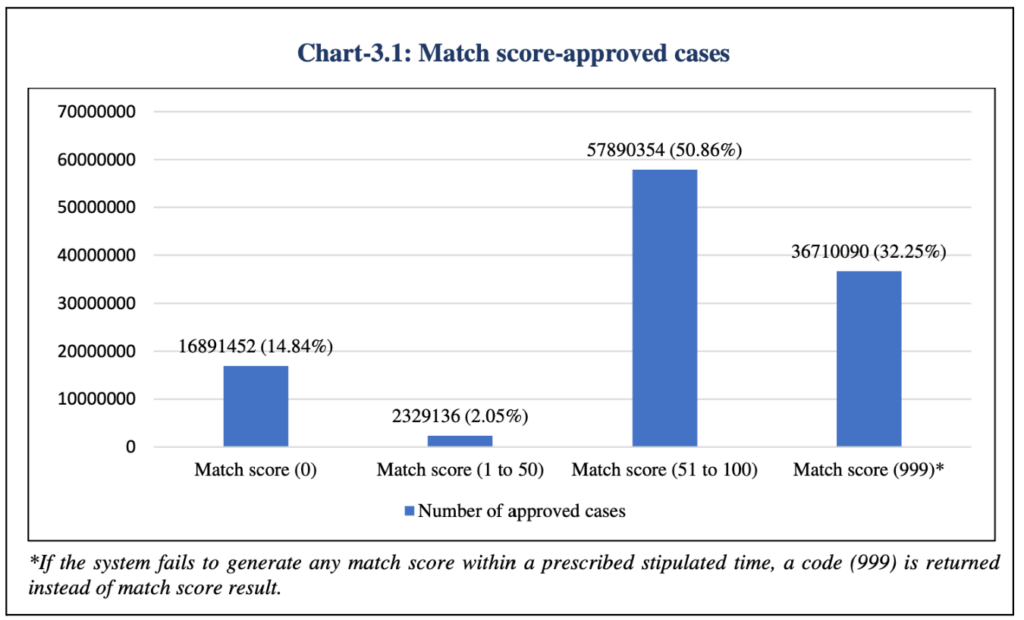
- No uniform threshold for Match confidence score which is used for approving or rejecting an application, which leads to ambiguity.
- Around 3.67 crores cases out of 11.38 crore approved cases did not fetch any match confidence score. Another 1.68 crore cases has the score as zero.
On the other hand, nearly 38.6 lakh cases out of 94.9 lakh rejected cases have a match confidence score in the range of 51-100.
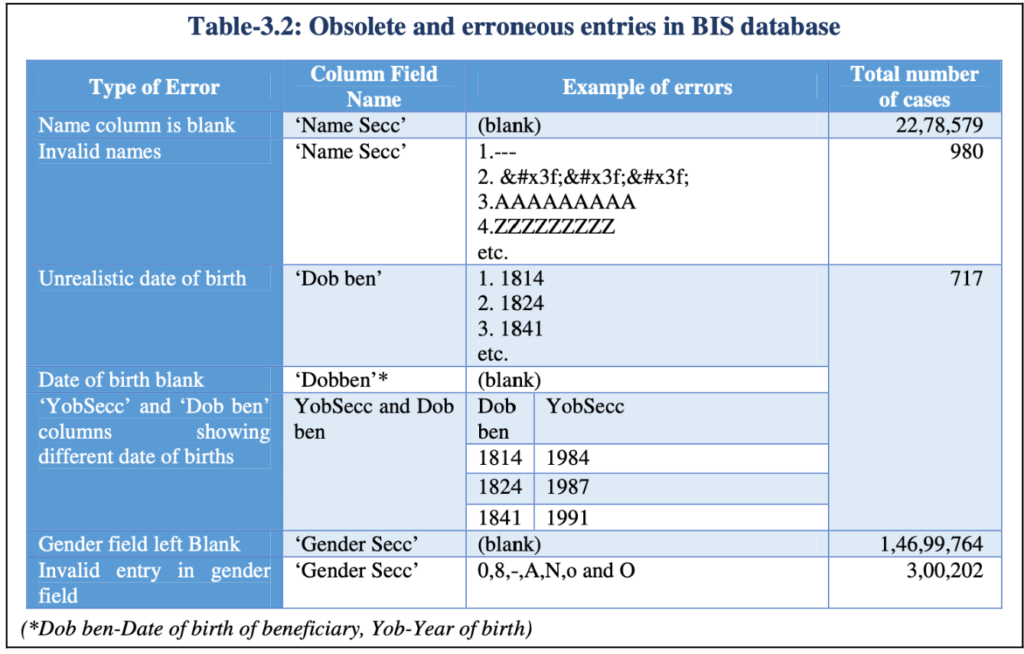
CAG report also raised apprehensions about the quality of the data available in the Beneficiary Identification System (BIS) Database. One of the concerns was that the data available was for 2011. By 2018, there could have been changes to the status of the families i.e., few would no more be eligible, and few others are newly eligible, making the data obsolete. It also highlighted the concern with erroneous data.
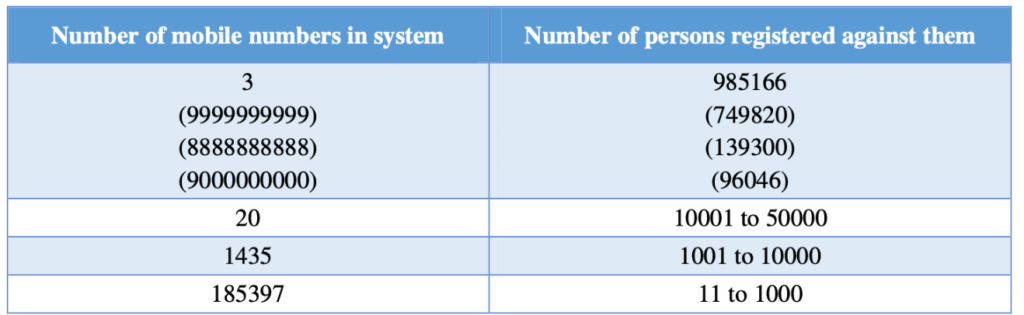
Registration of multiple beneficiaries against same or invalid mobile numbers
Each verified eligible beneficiary is assigned a PMJAY ID and serves a unique identification key. Data analysis as part of the audit revealed that PMJAY ID is not unique in 1.57 lakh approved cases. Among them, in more than 1.05 lakh cases PMJAY ID is appearing twice.
This presence of duplicate IDs indicates the possible presence of ineligible beneficiaries in the database. Data analysis highlighted further inconsistencies:
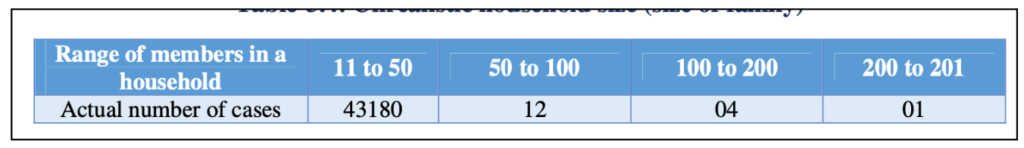
- For more than 43 thousand households, the family size was unrealistic ranging from 11 to 201 members. This not only indicates a lack of validation controls but also the possibility that beneficiaries are taking advantage of the lack of a clear definition of family in the guidelines.
In Tamil Nadu, 4761 PMJAY cards were mapped to multiple Aadhar numbers.
Guidelines indicate that a contact number will be used for any communication related to the scheme. Analysis of the database indicates large numbers of beneficiaries have registered against the same or invalid mobile numbers. Overall, 1119 to 7,49,820 beneficiaries were linked with a single mobile number in the BIS database.
NHA has accepted these discrepancies highlighted by CAG and stated that these issues would be resolved with the deployment of BIS 2.0.
- The audit has also highlighted that across states, ineligible households are possessing PMJAY cards and also are availing treatment. Government employees, pensioners etc need to be excluded from the list of eligible beneficiaries. But is observed that in many states, they are part of the beneficiaries.
CAG also highlighted discrepancies in Hospital empanelment, claims management etc.
Apart from the inconsistencies in the beneficiaries of PMJAY, the CAG audit also highlighted issues with the implementation of the scheme in various other areas including Hospital empanelment, claims management, Finances, etc. Here is a snapshot of a few of these issues highlighted.
- In several States, the hospitals empanelled were found to have shortage of infrastructure, equipment, doctors etc. Mandatory compliance criteria for empanelment of hospitals relating to infrastructure, safety measures, bio-medical waste management, pollution control etc were not met.
- Physical verification was not conducted in 163 EHCPs in Manipur (17), Tripura (103) and Uttarakhand (43).
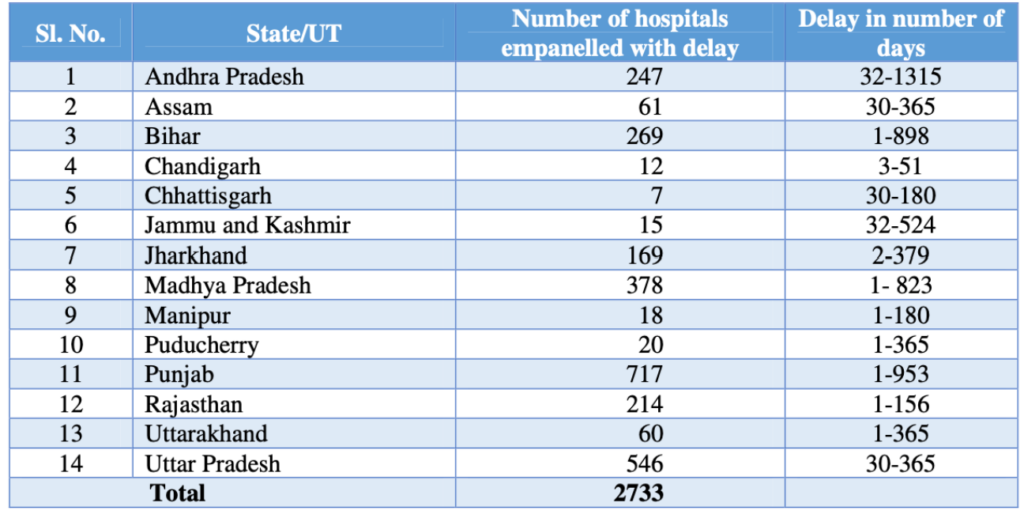
- Empanelling a hospital needs to complete in 30 days, but 2733 hospitals were empanelled with a delay.
During 2018-19, NHA released grant amounting of Rs. 185.6 crores to eight States without ensuring release of upfront shares by the respective States. NHA has also released grants in three different bank accounts to Chhattisgarh during 2018-21.
In 20 State Health Authorities (SHA), administrative grant of around Rs. 368 crores remain unspent during 2018-21.
District Implementing Units (DIUs) were not formed in five states. There is shortage of manpower in 22 states for various posts in SHAs and DIUs.
Only 9.8% of the complaints received were redressed within the turnaround time.
Strengthening the validation process, investing in infrastructure among the recommendations.
CAG made various recommendations for improving the implementation of the scheme. Here are a few important recommendations.
- To have a suitable mechanism in place for identifying State-wise beneficiaries under the scheme and to weed out ineligible beneficiaries in a time-bound manner.
- Validation checks should be in place to avoid invalid entries and increase the accuracy and reliability of the data.
- NHA must put in a mechanism to map and identify PMJAY beneficiaries so that there is no overlap of PMJAY and state specific schemes.
- Need to invest in public hospitals to improve and upgrade the quality of the existing healthcare facilities. Encourage private hospitals to be part of the scheme.
- Monitoring of EHCPs through physical inspections and necessary audits so that mal practices may get detected and action may be initiated.
- SHAs must ensure that claim amount is utilized by Public/Government Hospitals for improving the overall infrastructure, functioning of the hospital etc.
- Diversion of grant from one head to another should be discouraged and NHA/SHA should ensure that grant is utilized for the purpose it was released.
More than 24.51 crore Ayushman Cards created
As per AB-PMJAY dashboard, more than 24.5 crore Ayushman cards were created so far. In the last 30 days, more than 30 lakh cards were created. The highest number of Ayushman cards are in Madhya Pradesh with around 3.63 crores followed by Uttar Pradesh and Chhattisgarh.
Overall, 27.7 thousand hospitals are empanelled of which 15.6 thousand are public hospitals. The dashboard indicates that since the introduction of the scheme, there were around 5.5 crores authorised hospitalisations. Tamil Nadu has recorded the highest number of hospitalizations followed by Karnataka and Rajasthan.
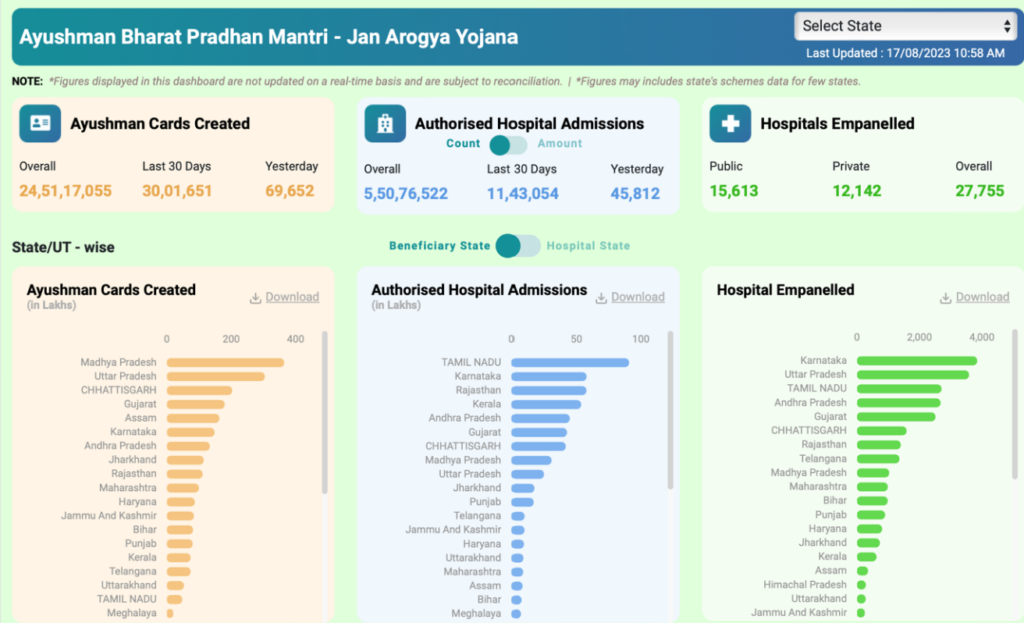
Around 4.7 thousand empanelled hospitals are inactive since empanelment and a further 3.6 thousand were identified as inactive since the past 6 months. The highest number of hospitals inactive since empanelment are in Andhra Pradesh. In fact, 46% of the hospitals empanelled in Andhra Pradesh are inactive since the beginning.
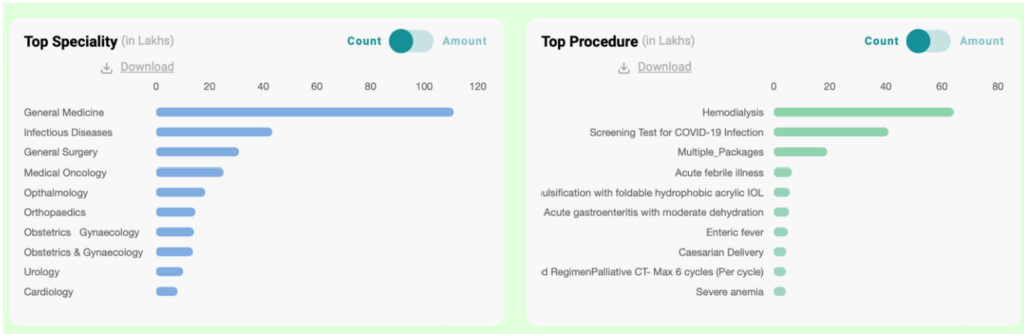
Data indicates that PMJAY was mostly utilised to cover the procedure of Haemodialysis followed by screening test for COVID-19 infection. General Medicine and Infectious diseases top the list of specialties for which PMJAY was utilised.
Featured Image:AB-PMJAY Dashboard