As the world races towards launching a COVID-19 vaccine for public use, clinical trials and their impact on participants have caught the attention of people. Data from the government indicates that between 2015 & September 2020, about 176 deaths related to clinical trials were reported in India.
As the coronavirus pandemic spread globally, scientists and organizations from different parts of the world started dedicating their time and resources towards finding a cure and vaccine to fight the virus. Thanks to the medical research in the last few months, there has been a significant improvement in the knowledge regarding the virus and the disease, compared to what was known during early 2020. The research helped to a great extent in finding a treatment protocol among other things. As organizations rush to complete the clinical trials and bring them out for public use, there is a need to understand what happens in these clinical trials and how adverse events are taken care of, especially in India. Here is a detailed story.
Multiple stages need to be passed before a vaccine or a drug is approved for public use
For the development of drugs and vaccines, there are multiple stages of medical research which the drug/vaccine must pass through, following which it is reviewed and rolled out for larger public use. The New Drugs and Clinical Trials Rules, 2019 governs these practices. The initial stage of discovery and development, known as the non-clinical stage, is that phase when compounds that help in treatment, dosage, effectiveness, toxicity, and interaction with other drugs and treatments, are studied. The details like the effect the drug has on animals and how it demonstrates therapeutic potential for humans must be specified. Clinical trials follow this stage.
Factors such as safety, reaction, and tolerance need to be recorded during Clinical Trials
The clinical trials rules of 2019 define clinical trial as any systematic study of new drug, performed in people to evaluate the drug or the medical intervention for safety, tolerance, and effectiveness. For instance, how harmful are the side effects of the intervention is studied at this stage. There are four different phases in which clinical trials are carried out. In each phase, the results obtained in the preceding phase are reviewed and used. The population size in each phase increases and the composition diversifies as the trials advance to the next phase. These are-
Phase I– Drug activity, the drug’s absorption, distribution, metabolism, and excretion, dosage is measured, observed, and monitored while using the drug on healthy individuals or certain types of patients.
Phase II– A group of patients based on certain criteria, a relatively homogenous population, are selected for carrying out this phase of trials, during which the dose and regimen for the next phase is determined.
Phase III– This is the stage when the demonstration and confirmation of therapeutic benefits happens. Large scale trials take place at this stage with thousands of subjects depending on the type of drug/vaccine. Information pertaining to usage of drug/vaccine is gathered in this stage.
Phase IV– Also known as post marketing trial, this phase of trials is usually performed after the drug gets approval. Additional drug-drug interaction, safety studies, dose response, mortality and morbidity studies, etc. are covered in this phase.
Participation in human trials is voluntary and informed consent is mandatory
For any person to participate in clinical trials, it is important that the investigator obtains an informed consent in writing from the participant or guardian, in case of children. For this, the investigator must clearly provide details of the study to the participant both verbally and in writing in a simple, non-technical language. It is also mandatory that all clinical trials being carried out in the country register themselves with the Clinical Trial Registry of India, maintained by the ICMR, even before the first participant gets enrolled. An Ethics Committee is constituted that constantly reviews the ongoing research. Strict compliance with the rules must also be ensured.
The Clinical Trial Registry website comes with an option to search for information about trials that have been registered with them. Here is a screenshot of the webpage.
Registration of clinical trials is important as it helps in making the research more transparent and keeps a check on publication bias and selective reporting. Moreover, it is the lives of people at stake when a clinical trial is carried out. However, pharmaceutical companies refrain from registering for fear of their intellectual property getting stolen.
Serious Adverse Events such as death or impairment should be informed to the Central Authority
In case any new drug/vaccine results in death, permanent disability, congenital anomaly, or any other life-threatening event in a participant during the clinical trials, the trials are then paused to understand the reason for such an impact. Such an instance, or ‘Serious Adverse Event (SAE)’, has been described as follows in the latest Drugs and Clinical Trials Rules.
‘an untoward medical occurrence during clinical trial resulting in death or permanent disability, or hospitalisation of the trial subject where the trial subject is an outdoor patient or a healthy person, prolongation of hospitalisation where the trial subject is an indoor-patient, persistent or significant disability or incapacity, congenital anomaly, birth defect or life threatening event’
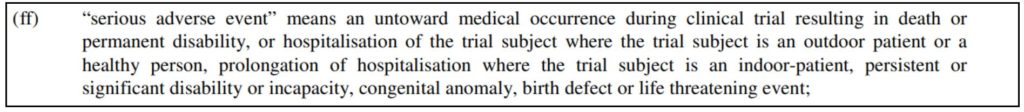
Since the trial is carried out on people as an experiment, the results may not be as expected and can cause a SAE. In such cases, the investigators must report the event to the Central Licensing Authority (CLA) and the Ethics Committee within 24 hours. The CLA will constitute another expert committee to examine the case, in case of a death, and provide recommendations with respect to cause of death and quantum of compensation. The Ethics Committee investigates the matter in case of injury and proposes the final compensation.
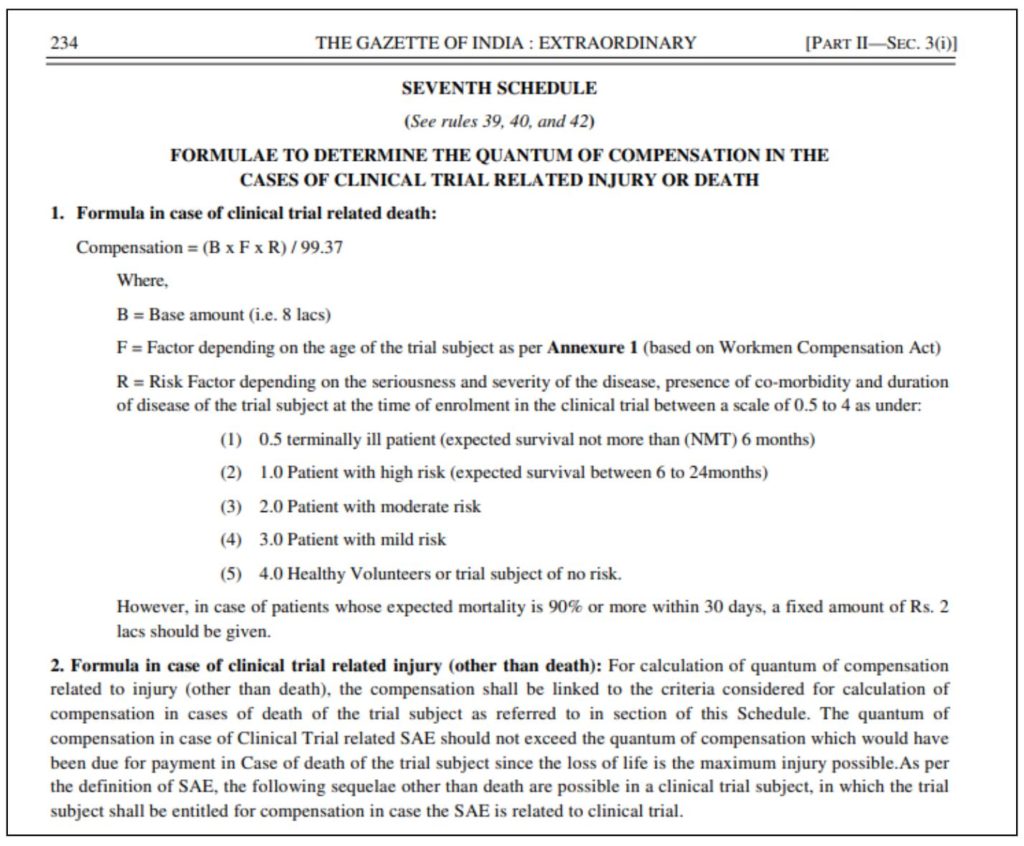
Compensation is calculated by a Committee based on formulae
The compensation in case of a SAE is calculated on the basis of base amount, age factor of participant, and the risk factor depending on seriousness of disease, comorbidities, and duration of disease. The base amount is Rs. 8 Lakhs. Age factor ranges from 228.54 for the age of 16 to 99.37 for those aged 65 years and above. The risk factor also varies between 0.5 to 4. For those whose mortality is expected to be 90%, a compensation of Rs. 2 lakhs have been fixed. For events of injury, the compensation should not be more than that in case of death.
From 2015 to 09 September 2020, a total of 176 SAEs of death related to clinical trials have been reported in India, out of which, compensation was paid in 156 cases. In total, Rs. 13.85 crore has been paid to the 156 families, an average of Rs. 8.88 Lakh per person. During the same period, six cases of illegal clinical trials were registered, as per government’s response in the Lok Sabha.
Past instances of illegal clinical trials in India have resulted in many deaths
In March 2010, there were media reports of female children and adolescents having died in Khammam District in Andhra Pradesh after being administered Human Papilloma Virus (HPV) vaccines, trials of which were being carried out by Programme for Appropriate Technology in Health (PATH) reportedly funded by the Bill and Melinda Gates Foundation. A parliamentary Standing Committee report tabled in May 2013 stated that there was ‘serious dereliction of duty’ by the institutions and individuals involved. They further accused the department of acting in favour of drug manufacturers by giving a nod for marketing the drugs in India instead of conducting clinical trials here. Another report highlighted that between January 2008 and October 2010, around 31 new drugs were approved in India without conducting clinical trials. There was no scientific evidence or data backed evidence for the usage of these drugs in India. This could have potentially resulted in harm to public health. There are numerous reports from the past which throw light on how illegal trials were being conducted in India. The rules brought about in 2019 was an effort to ensure registration and make the system transparent in the country.
Clinical Trials for COVID-19 Vaccine are being conducted in India
Currently, three vaccine trials on humans for COVID-19 are being conducted in India. These are-
- COVAXIN – Developed by Bharat Biotech in collaboration with ICMR and National Institute of Virology. This India’s indigenous vaccine is currently in Phase II of Human Clinical Trial.
- COVISHIELD – This vaccine is also in Phase II of human trials in India, which is being conducted jointly by Serum Institute of India and ICMR.
- ZyCOV-D has also entered Phase II of human trials in India
The list of all potential ‘Repurposed Drugs’ that can be used for COVID-19, where the Council of Scientific & Industrial Research (CSIR) is partnering in clinical trials is now available on the CSIR website.
Featured Image: Clinical Trials Serious Adverse Events


