[orc]Ever since the National Medical Commission bill was passed by both houses of Parliament, the medical fraternity, primarily doctors have been protesting against the various provisions of the act. One of them is the concept of Community Health Providers. Do the numbers justify the need for a CHP system?
This month witnessed a nation- wide protest by doctors and medical students following the approval of the National Medical Commission bill (NMC) in both the houses of parliament. In an earlier story on Factly, details of the National Medical Commission Act including the changes proposed, pros and cons have been discussed. In this story, we discuss the Community Health Providers (CHPs) as provided in the NMC and if the numbers justify the move towards introduction of CHPs.
Data provided by the Ministry of Health and Family Welfare (MoHFW) in the Lok Sabha indicates that there are 11.59 lakh registered allopathic doctors in India as on 31 March 2019. The Ministry further stated, supposing that the availability is 80%, there will be approximately 9.27 lakh doctors in India who may be available for active service. Since the population of India is a staggering 1.35 billion, the doctor population ratio is 1:1456, implying that there is one doctor for every 1456 people in the country. As per the recommendations of the World Health Organisation, the ideal doctor population ratio for a country is 1:1000 and India lags behind the WHO norm. India would need around 5 lakh more doctors to meet the WHO norms.
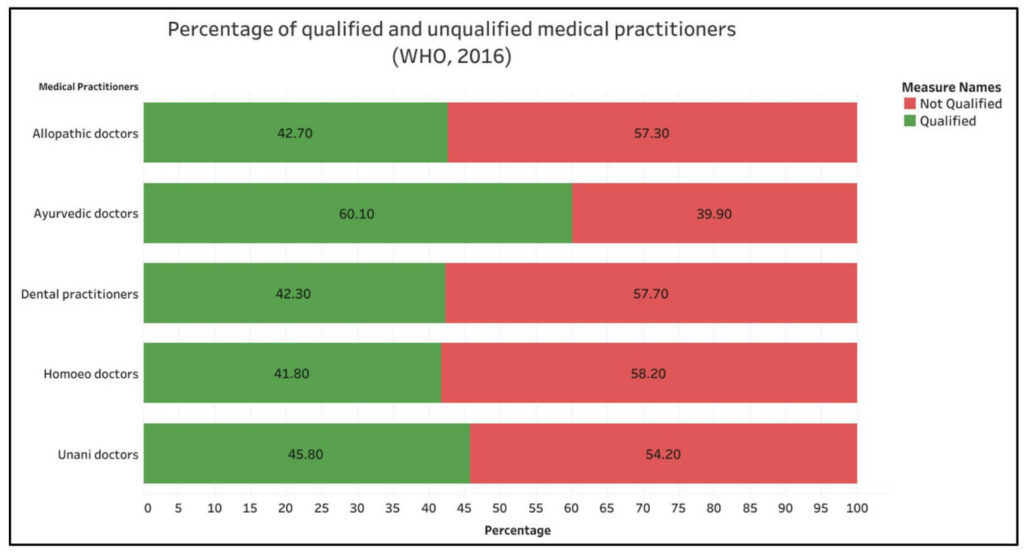
57.3% of the allopathic doctors in India do not possess a medical qualification as per a WHO report
As per a report on the Health Workforce in India published by WHO in 2016, of the total allopathic doctors in India, 57.3% of them did not possess a medical qualification. This study was conducted on the basis of the 2001 census data. The findings of the study were initially not accepted by the government. In Lok Sabha, on 28 June 2019, when a question was raised regarding the unqualified doctors in the country, the Minister of State for Health and Family Welfare, Ashwini Kumar Choubey stated that, the report was ‘erroneous’. He justified his statement by adding that the minimum qualification for enrolling in the State Medical Register to become a registered medical practitioner is MBBS and so, all doctors should be qualified.
The Minister also mentioned that health is a State subject and so the responsibility to deal with fraudulent doctors and unqualified medical practitioners is that of the state governments. As per the Indian Medical Council Act of 1956, the offender was liable to pay a fine up to Rs.1000 and/or face imprisonment up to one year. The National Medical Commission Act has raised the penalty up to Rs. 5 Lakhs and/or one year imprisonment.
Contradicting this statement made in the Lok Sabha, on August 6, 2019, the press release on ‘FAQs on National Medical Commission (NMC) Bill’ by Press Information Bureau of India highlighted that, at present 57.3% of the personnel currently practicing allopathic medicine did not have any medical qualification. In other words, 57.3% of the allopathic doctors were ‘quacks’. The number has been used to support Section32 of the National Medical Commission Act which gives the commission the authority to grant limited license to CHPs. This press release makes it clear that the government accepts the numbers put forward by the WHO report.
The WHO report also states that 31.4% of the allopathic doctors possessed education qualification only up to secondary school level. Further, the education level was higher among urban doctors than rural doctors. A total of 58.4% of the urban doctors had a medical qualification whereas this is only 18.8% among the rural doctors. The study on health workforce has also revealed that 39.9% of Ayurveda doctors do not have a medical qualification. Among Homeo and Unani doctors, 58.2% and 54.2% respectively do not possess any form of medical qualification. In the case of dental practitioners, 57.7% do not possess medical qualification.
Number of doctors in Urban areas is almost four times that in Rural areas
The Government has also added that the distribution of doctors in rural and urban areas is highly skewed. The ratio of doctors in urban and rural areas has been stated as being 3.8:1. The WHO also reported in the study that there were 12.25 lakh (59.2%) health workers in urban areas which accounts for 27.8% of the population while there are 8.44 lakh (40.8%) health workers in rural areas where the remaining 72.2% of the population resides. Health workers include doctors, nurses, mid-wives and ancillary health professionals. The government’s press release states that this disparity has resulted in the rural population falling prey to quacks. The reasons behind the dependence of rural and impoverished population on quacks are both access and affordability of healthcare.

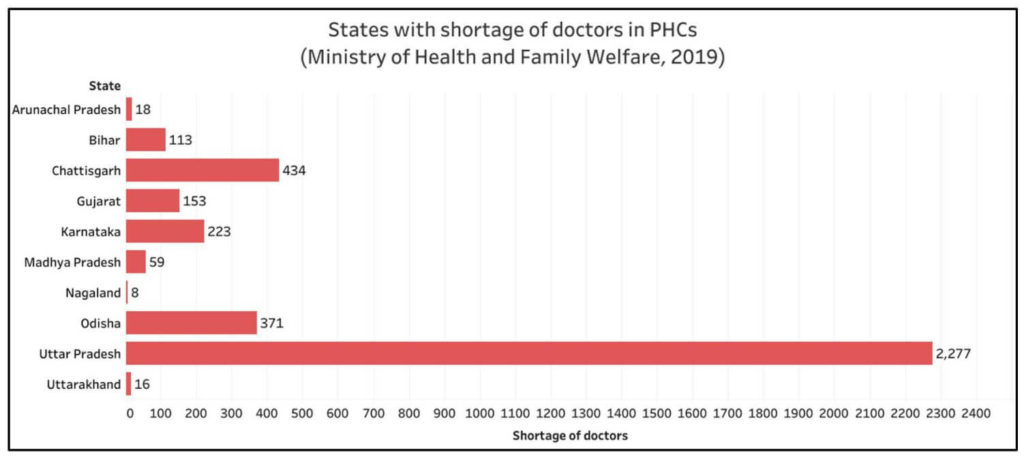
Shortage of 14.3% of doctors with respect to requirement in PHCs
In the Lok Sabha, MoHFW also provided data on the availability of allopathic doctors in Public Health Centres (PHCs) as on 28 June 2019. There is a shortage of 3,673 doctors across the country- a shortfall of 14.3% as compared to the requirement. While there is a requirement of 25,473 doctors in total and even though there 27,567 doctors in position, as on 31 March 2019, the distribution is not uniform. The shortfall in availability of doctors is witnessed in the states of Arunachal Pradesh, Bihar, Chhattisgarh, Gujarat, Karnataka, Madhya Pradesh, Nagaland, Odisha, Uttarakhand and Uttar Pradesh. Of the 3,673 shortfall of doctors, Uttar Pradesh (in spite of including 841 AYUSH doctors) has a shortfall of 2,277 doctors followed by 434 in Chhattisgarh and 371 in Odisha. Further, 1494 PHCs in the country are functioning without a doctor as per 2018 data including 295 PHCs in Chhattisgarh alone.
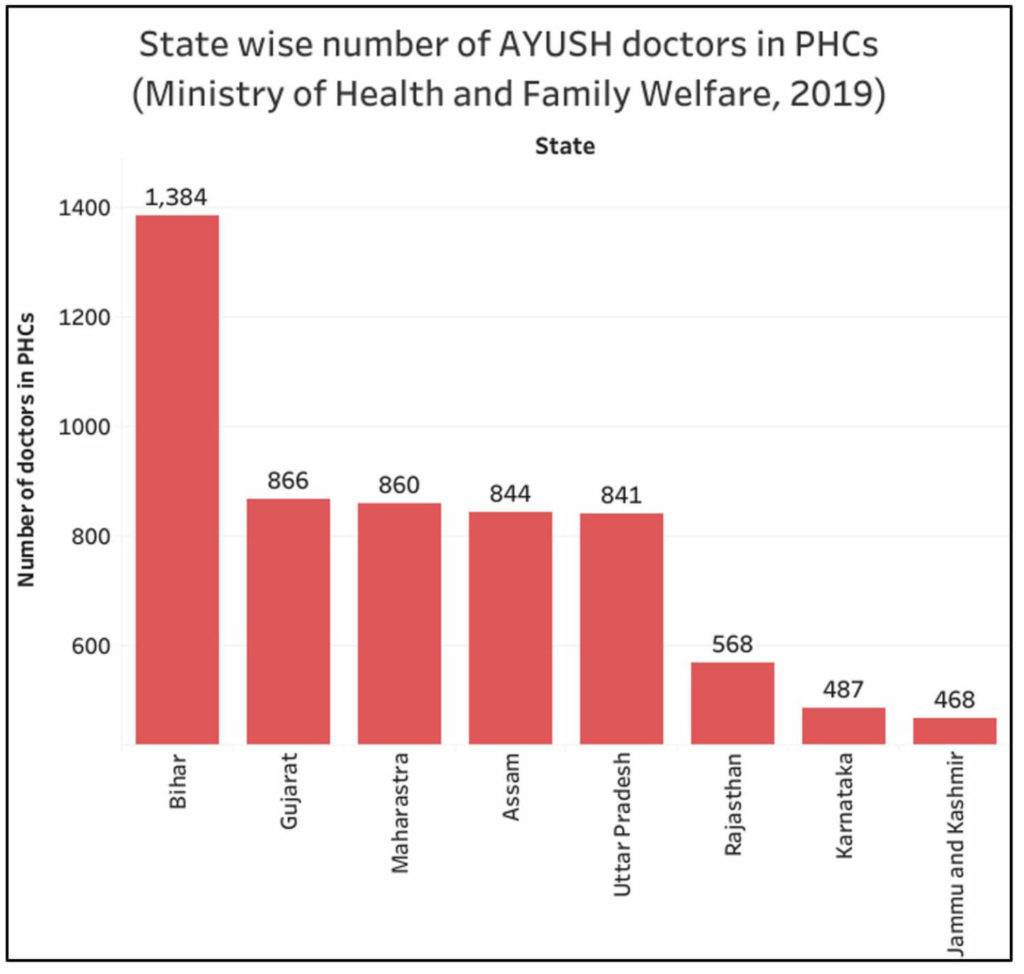
8860 AYUSH doctors have been appointed in PHCs in India
In the case of Ayurveda, Unani and Homeopath (AYUSH), the government reported that there are a total of 7.88 Lakh doctors of which, assuming 80% availability, approximately 6.30 lakh doctors available for service. If they are considered along with their allopathic counterparts, India’s doctor population ratio will be 1:867 which is much better than what is recommended by the WHO. The appointment of AYUSH doctors in PHCs comes under the purview of state governments. A total of 8860 AYUSH doctors have been appointed in PHCs in India with the 15.6% in Bihar (1384). The government mentioned in the Lok Sabha that co-location of AYUSH facilities at PHCs is to enable greater choice to the patients for different systems of medicine. The number of AYUSH doctors in PHCs is illustrated in the following chart.
Who are Community Health Providers?
According to the NMC act, Community Health Providers are those personnel who will be given a limited licence by the medical commission to practice medicine at mid-level. It should be someone connected to the modern scientific medical profession. The total number of CHPs should not exceed one third the total number of licensed registered medical practitioners under the National Register maintained by the Ethics and Medical Registration Board. The extent of their practice, circumstances and duration will be specified in the regulations. The CHPs are permitted to prescribe medicine independently in primary and preventive healthcare. However, in all other cases, they prescribe medicine only under the supervision of registered medical practitioners.
Similar initiatives in other countries have been found to be effective
In order to attain the government’s Ayushman Bharat objectives, there is a requirement for 1.5 lakh mid-level healthcare providers within the next 3 to 5 years. It would take another 7 to 8 years to fill this requirement purely by MBBS professionals considering the current level of medical education in India, Thus, to bridge this gap, other kinds of medical professionals like CHPs are a necessity for extending necessary healthcare. Further, the government has cited examples of such initiatives from other countries such as Thailand, United Kingdom and China where the outcomes have improved. The practice if done properly will also help relieve the medical practitioners from the existing overburden. It has been mentioned by the government that stringent regulations will be made with consultation of doctors for stipulation of norms for CHPs.
Considering the shortage of doctors in the country coupled with uneven distribution of the available doctors, CHPs can help in addressing this gap by attending to primary and preventive healthcare. While the government considers the inclusion of CHPs into healthcare as a measure to mitigate malpractice, medical practitioners are apprehensive as to this will lead to giving authority to quacks. Moreover, there are arguments that there are students who pass out of medical college and are unemployed. Introduction of CHPs will be a barrier for them since it increases competition for them. Since the regulations are yet to be formulated, not much is known about the norms to be set for CHPs in terms of qualification. However, the government would do well to take the medical community into confidence so that the CHP system does not lead to legitimizing quacks.
Featured Image: National Medical Commission bill



1 Comment
Thanks for sharing this information. your post helps me a lot.!!